What are ovarian cysts?
Ovarian cysts are fluid-filled sacs that can be found in one or both ovaries and are a common by-product of ovulation or an unsuccessful attempt at ovulation.
What causes ovarian cysts?
1. Hormone Imbalance
Hormonal imbalance is one of the most common causes of ovarian cysts. The ovaries rely on a delicate balance of hormones—especially estrogen, progesterone, LH (luteinizing hormone), and FSH (follicle-stimulating hormone)—to regulate ovulation. When this balance is disrupted:
- Follicles may not rupture properly, leading to follicular cysts.
- Ovulation may not occur at all, resulting in persistent cysts.
- Progesterone levels may be too low, preventing the proper breakdown of ovarian follicles.
Hormonal birth control, fertility drugs (like Clomid), or thyroid dysfunction can also contribute to cyst formation.
2. Stress
Chronic stress can interfere with the hypothalamic-pituitary-ovarian (HPO) axis, which regulates reproductive hormones. When under stress:
- The body may produce more cortisol, a stress hormone, which can suppress gonadotropin-releasing hormone (GnRH).
- This suppression can lead to irregular or missed ovulation, increasing the risk of functional ovarian cysts.
- Stress can also exacerbate hormonal imbalances already present from other causes.
While stress alone may not directly cause cysts, it can be a significant contributing factor—especially when combined with other underlying issues.
3. Endometriosis
Endometriosis is a condition in which tissue similar to the lining of the uterus grows outside of it. When this tissue implants on the ovaries:
- It can form endometriomas, also known as chocolate cysts, due to the presence of old, dark blood inside them.
- These cysts are often painful and can interfere with ovarian function and fertility.
- Unlike functional cysts, endometriomas do not go away on their own and often require medical or surgical treatment.
Endometriosis-related cysts are more common in women with chronic pelvic pain or a known history of the condition.
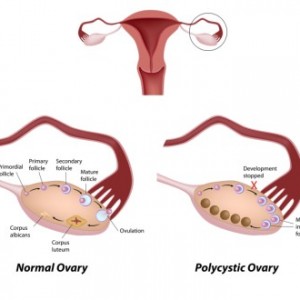
4. Polycystic Ovary Syndrome (PCOS)
PCOS is a hormonal disorder characterized by:
- High levels of androgens (male hormones) on blood work or clinical signs of high male hormones like acne, hirsutism, and hair loss,
- Irregular or absent ovulation and/or
- Small cysts on the ovaries, often described as a “string of pearls,” on ultrasound.
The “cysts” in PCOS are actually immature follicles that fail to ovulate due to hormonal imbalances. Unlike other types of cysts, they are not typically painful, but their presence reflects an ongoing issue with ovulatory dysfunction.
PCOS-related cysts are chronic and recurring and are associated with metabolic issues like insulin resistance and inflammation.
Are there different types of cysts?
Yes. The most common cysts are called functional cysts. These are benign and are one of two types:
- Follicular cysts – as an egg is developing it is encased in a follicle. Normally around mid-cycle the follicle opens and releases the fully developed egg. If it fails to release the egg, it may stay on the ovary as a cyst.
- Corpus Luteum cysts – after releasing the egg, the residual egg follicle becomes a progesterone-secreting structure called the corpus luteum. This is normal. Sometimes, the corpus luteum closes up into a sac and becomes a cyst. These usually resolve on their own, but they can bleed, twist the ovary or cause pain.
Other types of ovarian cysts include:
Endometriomas:
Endometriomas are cysts of endometriosis on the ovaries. They are the rare occasion when endometriosis can be seen on ultrasound.
Hemorrhagic Cysts:
A hemorrhagic cyst is a functional ovarian cyst that occurs when a blood vessel within the cyst wall breaks, causing bleeding into the cyst itself. These cysts typically form from a corpus luteum, the structure left behind after ovulation.
Key Features of Hemorrhagic Cysts:
Painful: The bleeding can stretch the ovary or irritate surrounding tissues, often causing sudden, sharp pelvic pain on one side.
Self-resolving: In many cases, hemorrhagic cysts resolve on their own within a few weeks without treatment.
Ultrasound findings: They often appear with characteristic patterns like a “lace-like” or “cobweb” appearance on imaging.
Rupture risk: If a hemorrhagic cyst ruptures, it can cause internal bleeding, which may require emergency medical attention.
Dermoid Cysts (Mature Cystic Teratomas):
A dermoid cyst is a benign (non-cancerous) ovarian tumour that develops from embryonic cells. These cells are capable of forming various types of body tissues, so dermoid cysts often contain fully formed structures such as:
- Hair
- Teeth
- Skin
- Fat
- Occasionally, cartilage or even bone
Key Features of Dermoid Cysts:
Present from birth: Dermoid cysts are congenital, meaning they are present from birth but may not be discovered until adolescence or adulthood.
Slow-growing: They tend to grow slowly and are often found incidentally during pelvic exams or imaging.
Usually painless: Many dermoid cysts cause no symptoms unless they become large, rupture, or twist the ovary (ovarian torsion), which is a medical emergency.
Require removal: Because they are solid and do not resolve on their own, dermoid cysts are typically surgically removed, especially if they are large or symptomatic.
Do cysts need to be surgically removed?
Not usually. Most cysts will go away on their own. Having an ovarian cyst is rarely an emergency. Cysts that may require surgery include:
- Hemorrhagic cysts that are causing significant blood loss and anemia.
- Cysts that cause significant pain that cannot be controlled with over-the-counter medication.
Does having an ovarian cyst mean I have PCOS?
Not necessarily, but if you have other symptoms of PCOS (irregular periods, excessive facial hair, acne, head hair loss, infertility, acanthosis nigricans) and an ovarian cyst, that possibility should be thoroughly investigated with PCOS tests and ruled out.
Does having cysts mean I am infertile?
Not necessarily, although the conditions that caused a cyst to form may also contribute to infertility. Two conditions that contribute to cyst formation and that are associated with most female fertility problems are endometriosis and Polycystic Ovarian Syndrome (PCOS).
What is the naturopathic treatment for ovarian cysts?
As with anything with naturopathic medicine, we address the condition’s root cause. There are a variety of natural treatments to restore healthy hormone balance and to treat endometriosis and PCOS.
For help with this or any other health problem, book an appointment here or call the office for more information at 416-481-0222. I can give you tailored advice in person or virtually if you are anywhere in Ontario. If you are elsewhere, I can’t provide personalized treatment, but you can get general information about natural approaches for PCOS in my ebook here.
by Dr. Pamela Frank, BSc(Hons), ND
Dr. Pamela has practiced as a naturopathic doctor in Toronto since 1999. She has received numerous “Best Naturopath in Toronto” awards. She is registered with the College of Naturopaths of Ontario.
Dr. Pamela Frank uses a natural treatment approach that may include acupuncture, herbal medicine, nutrition, diet, vitamins, supplements, and other natural remedies to restore balance and provide long-term resolution to almost any health problem.
