When it comes to diagnosing and managing polycystic ovary syndrome (PCOS), there’s no shortage of opinions and no shortage of lab testing for PCOS you could do. But more testing isn’t always better. Some commonly ordered labs offer little value for diagnosis or treatment, while others are essential for understanding the root causes and guiding care.
This guide takes an evidence-informed approach rooted in current research and clinical guidelines to help you understand which lab tests matter most for PCOS, and which you can safely skip.
First, a Quick Reality Check
- There’s no single blood test for PCOS.
- Diagnosis is based on a combination of symptoms, physical findings, and lab results (the Rotterdam criteria being the most widely used).
- Lab testing for PCOS plays two key roles:
- Ruling out other causes of irregular cycles or infertility
- Assessing underlying metabolic and hormonal imbalances
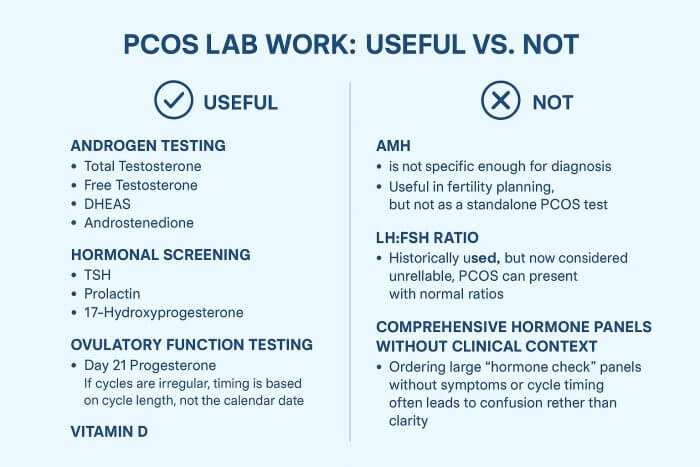
The Most Useful Lab Testing for PCOS
1. Thorough Androgen Testing (for Excess Testosterone)
High androgens are a hallmark feature in many—but not all—people with PCOS.
- Total Testosterone – Best initial screen for androgen excess
- Free Testosterone – More sensitive if total is normal but symptoms are present
- DHEAS (Dehydroepiandrosterone Sulphate) – Helps determine if excess androgens are coming from the adrenal glands
- Dihydrotestosterone – This ultra-potent testosterone can be elevated when other androgens are normal
- Androstenedione – Sometimes useful as an additional androgen marker
Why it matters: Elevated androgens contribute to irregular periods, infertility, acne, hair thinning, and excess facial/body hair, and guide treatment choices.
2. Hormonal Screening to Rule Out Other Conditions
Symptoms of PCOS can mimic other endocrine disorders. Ruling these out prevents misdiagnosis.
- TSH (Thyroid-Stimulating Hormone) – Screens for hypothyroidism or hyperthyroidism
- Prolactin – High levels may indicate a pituitary disorder
- 17-Hydroxyprogesterone – Rules out non-classic congenital adrenal hyperplasia (NCAH)
3. Ovulatory Function Testing
- Day 21 Progesterone (or 7 days before expected period) – Confirms if ovulation is occurring. If cycles are irregular, timing is based on cycle length, not the calendar date.
4. Metabolic Health Assessment
PCOS increases the risk of insulin resistance, type 2 diabetes, and cardiovascular disease—often regardless of body size.
- Fasting Glucose and Fasting Insulin
- Oral Glucose Tolerance Test (OGTT) – Gold standard for detecting insulin resistance
- Lipid Panel – Checks cholesterol and triglycerides
- HbA1c – Reflects average blood sugar over 3 months
Why it matters: Even in young, lean individuals with PCOS, metabolic issues are common.
5. Vitamin D
While not diagnostic for PCOS, deficiency is common and may impact insulin sensitivity, inflammation, and reproductive health.
Tests with Limited Diagnostic Value in PCOS
AMH (Anti-Müllerian Hormone)
While AMH tends to be higher in PCOS, it’s not specific enough for diagnosis.
Useful in fertility planning, but not as a standalone PCOS lab test.
LH:FSH Ratio
Historically used, but now considered unreliable.
PCOS can present with normal ratios, and many without PCOS have elevated ratios.
Comprehensive Hormone Panels Without Clinical Context
Ordering large “hormone check” panels without proper cycle timing often leads to confusion rather than clarity.
How to Approach Lab Testing for PCOS
- Start with a straightforward clinical question – Is this for diagnosis, ruling out other causes, or tracking treatment progress?
- Time the tests appropriately – Hormones like estrogen and progesterone vary significantly through the menstrual cycle. Measuring progesterone prior to expected ovulation is useless information.
- Interpret results in context – Labs are only one piece of the puzzle and lab ranges are not set based on optimal or ideal levels. That’s my target.
Bottom Line on Lab Testing for PCOS
The proper lab testing for PCOS is targeted, purposeful, and interpreted in context. Too often, people are left with long, expensive lab lists that add little to diagnosis or treatment. Working with a naturopathic doctor who understands both the diagnostic criteria and the latest evidence ensures that you get meaningful results—without unnecessary tests.
✅ If you have PCOS or suspect you might, I help patients understand their lab results, identify the root causes of their symptoms, and create personalized, evidence-based treatment plans. Book a consultation here.