If you’ve heard that PCOS is only about your ovaries, think again. One of the most common and misunderstood drivers of PCOS is insulin resistance. And it often starts before symptoms like irregular periods or acne ever appear.
What Is Insulin Resistance?
Insulin is the hormone that helps move sugar from your blood into your cells for energy. When your cells stop responding well to insulin, your body produces more of it to compensate.
Over time, high insulin levels can:
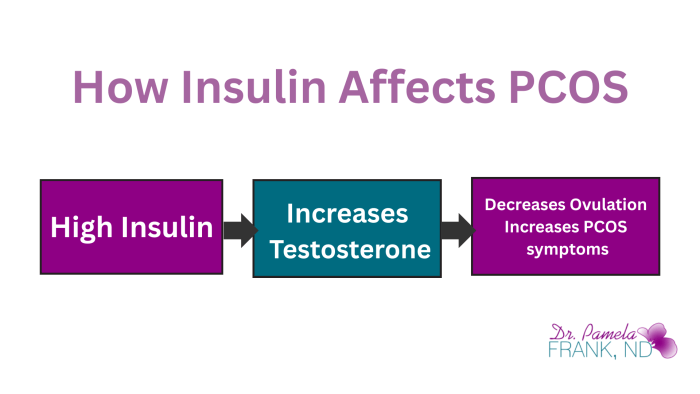
- Trigger the ovaries to produce more testosterone and/or dihydrotestosterone and/or the adrenal glands to produce more DHEA and androstenedione. These increased male hormones then disrupt the ovulation process.
- Contribute to inflammation and fatigue.
- Lead to weight gain, especially around the belly. Insulin’s job is to move sugar from the blood into cells and tell your body to store that sugar as fat.
Why Insulin Resistance Matters in PCOS
Research shows that up to 70% of people with PCOS have some degree of insulin resistance, even if their blood sugar looks “normal.” You can have a normal amount of sugar in your blood, but make copious amounts of insulin to maintain that normal sugar level.
Insulin doesn’t just regulate sugar. It talks to your reproductive system.
High insulin levels can disrupt the brain-ovary communication that regulates your menstrual cycle.
Signs of Insulin Resistance You Might Miss
You don’t have to be overweight or have diabetes for insulin resistance to be a problem. Some signs include:
- Intense carb or sugar cravings
- Midsection weight gain (even with exercise)
- Fatigue after meals
- Acne or oily skin
- Skin tags or dark patches known as acanthosis nigricans (especially on the neck or underarms)
- And obviously, PCOS.
What Can Help Insulin Resistance?
Managing insulin resistance usually requires a multi-pronged approach:
- Balanced blood sugar through nutrition
- Daily movement, particularly cardio or HIIT workouts
- Stress management (because cortisol affects blood sugar and insulin, too)
- Good sleep hygiene. Even one night of less than 5 hours of sleep leaves you more insulin resistant the next day.
- Supportive nutrients (as assessed by your practitioner)
How Can You Measure Insulin Resistance?
There are several options to measure your blood sugar and insulin levels. The most basic of tests is your fasting blood sugar level. This, in my view, is the worst indicator of insulin resistance. If your blood glucose level is still high twelve hours after you last ate, you are very far gone at that point. You are very insulin resistant and you are diabetic at that point. We would prefer to pick up insulin resistance before your fasting blood sugar becomes abnormal.
You can measure a fasting insulin level. Again, if your insulin level is still high twelve hours after you last ate, you are very insulin resistant.
My preferred test for insulin resistance is a test called an Oral Glucose Tolerance Test WITH Insulin Measurements. What we are trying to do with this test, is challenge your body with a set amount of sugar and gauge how much insulin your body has to make to deal with that amount of sugar.
How the test is performed, is that you would go to the lab after fasting for twelve hours. The lab will draw a fasting sample. I would order a fasting glucose AND a fasting insulin level. If the fasting glucose is normal, the lab will give you a VERY sugary drink that contains 75 grams of sugar. Then I would order a glucose and insulin measurement one hour and two hours after the drink.
This tells us not only are you able to return your blood sugar level to normal within two hours of this glucose challenge, but how much insulin did you have to make to do so. The level of insulin needed is what tells us if you are, or are not insulin resistant.
The Takeaway About PCOS and Insulin Resistance:
If you’re struggling with PCOS symptoms and not getting answers, ask about insulin resistance testing even if your glucose looks fine.
Managing insulin resistance often creates a ripple effect, resulting in improved energy, more regular cycles, and even clearer skin.
📥 Download the free Period Health Checklist to start tracking symptoms that may relate to insulin resistance.