Polycystic Ovary Syndrome (PCOS) is often thought of as a reproductive or fertility condition, but the effects reach far beyond irregular periods and difficulty conceiving. PCOS is a complex hormonal and metabolic condition that can increase the risk of several chronic diseases later in life.
Understanding PCOS and chronic disease risks is crucial because, with the right lifestyle changes, early monitoring, and targeted treatment, many of these long-term health issues can be prevented or mitigated.
PCOS and Insulin Resistance
One of the key drivers of long-term risk in PCOS and chronic disease is insulin resistance. Even women with a normal weight can experience it. Insulin resistance occurs when the body is unable to use insulin effectively, resulting in elevated blood sugar and insulin levels. Over time, this can increase the likelihood of:
- Type 2 diabetes
- Prediabetes
- Gestational diabetes during pregnancy
What you can do: Regular blood work (including fasting glucose, insulin, and HbA1c), strength training, balanced nutrition, and supplements such as inositol or vitamin D (when clinically appropriate) can all help improve insulin sensitivity.
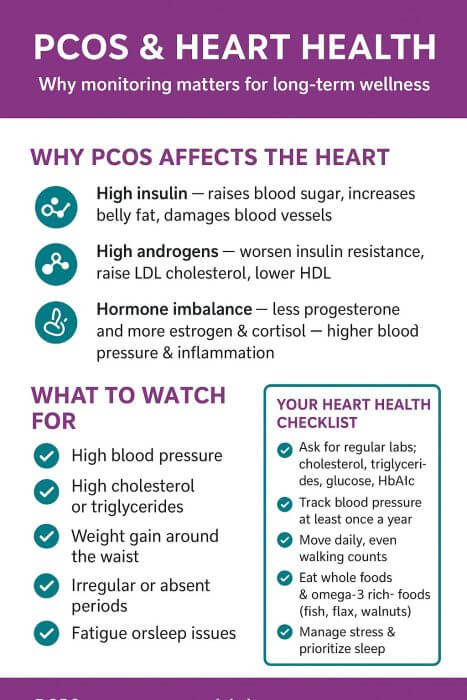
PCOS and Cardiovascular Disease
High insulin, elevated androgens, and hormonal imbalances in PCOS can all increase the risk of cardiovascular disease. These overlapping factors work together to affect blood vessels, cholesterol levels, blood pressure, and fat distribution throughout the body.
High Insulin and Insulin Resistance
Insulin resistance is common in PCOS, and when the body doesn’t respond appropriately to insulin:
- Blood sugar rises, damaging blood vessels and accelerating atherosclerosis (plaque buildup).
- Insulin levels remain high, promoting the storage of fat around the abdomen (visceral fat), which is strongly associated with an increased risk of heart disease.
- Inflammation increases, leading to oxidative stress and further injury to blood vessel walls.
- Liver cholesterol production changes, increasing triglycerides and LDL cholesterol while lowering protective HDL cholesterol.
Over time, this creates an ideal environment for the development of cardiovascular disease.
Elevated Androgens
High androgen levels (such as testosterone and DHEAS) don’t just affect hair and skin; they also impact heart health by:
- Worsening insulin resistance creates a vicious cycle.
- Promoting central obesity (weight gain around the waist), which carries higher heart risks than fat stored elsewhere.
- Altering vascular function, making arteries stiffer and less responsive.
- Influencing blood lipids, raising LDL cholesterol and lowering HDL cholesterol.
Hormonal Imbalances
Beyond insulin and androgens, other hormonal shifts in PCOS play a role in heart health:
- Low progesterone from irregular ovulation → Progesterone protects the blood vessels. Without it, that protection is lost.
- Excess estrogen without balance → Chronic “unopposed estrogen” increases inflammation and may affect vascular tone.
- Higher stress hormones (cortisol) → Elevated cortisol promotes abdominal fat storage, high blood pressure, and higher cholesterol.
The Bigger Picture about PCOS and Cardiovascular Disease
These combined changes often cluster together, creating what’s known as metabolic syndrome, a condition defined by high blood pressure, abdominal obesity, abnormal cholesterol levels, and increased inflammation. Metabolic syndrome significantly raises the risk of heart disease and stroke.
What you can do: Monitor blood pressure and cholesterol regularly, maintain an active lifestyle, reduce processed foods and added sugars, and prioritize omega-3–rich foods like fish, walnuts, and flaxseeds.
PCOS and Endometrial Cancer
PCOS is associated with irregular or absent ovulation. When ovulation doesn’t occur, progesterone levels remain low, but estrogen can stay normal to high, creating a state of “unopposed estrogen.” Over time, this can increase the risk of endometrial hyperplasia (thickening of the uterine lining) and, in some cases, endometrial cancer.
What you can do: Track your menstrual cycles, work with your doctor to ensure regular shedding of the uterine lining (through lifestyle, herbs, supplements, or medications if needed), and seek medical advice if you have prolonged irregular bleeding or missed periods.
PCOS and Mental Health
Chronic health risks aren’t only physical. PCOS is linked with higher rates of:
- Depression and anxiety
- Body image concerns
- Sleep disturbances, including sleep apnea
These factors can compound physical risks and make lifestyle changes more difficult.
What you can do: Support mental health through stress management, adequate sleep, social support, and professional counselling when needed. Addressing both the emotional and physical aspects of PCOS leads to better overall outcomes.
Key Takeaways About PCOS and Chronic Disease
PCOS is not just about periods or fertility; it’s a lifelong condition with significant health implications. PCOS and chronic disease are intertwined. The good news is that early and proactive care can make a considerable difference. By monitoring key risk factors and making sustainable changes, you can significantly reduce your chances of developing chronic disease.
Practical next steps for PCOS and chronic disease risk:
- Ask your doctor for regular screenings (including blood sugar, insulin, HbA1c, cholesterol, blood pressure, and hormone levels).
- Track your cycles and symptoms.
- Prioritize movement, whole foods, and sleep.
- Seek personalized support from a naturopathic doctor experienced in PCOS.
Remember: PCOS and chronic disease risk are real, but it does not define your future health. With the right tools, you can take control and lower your long-term risks.