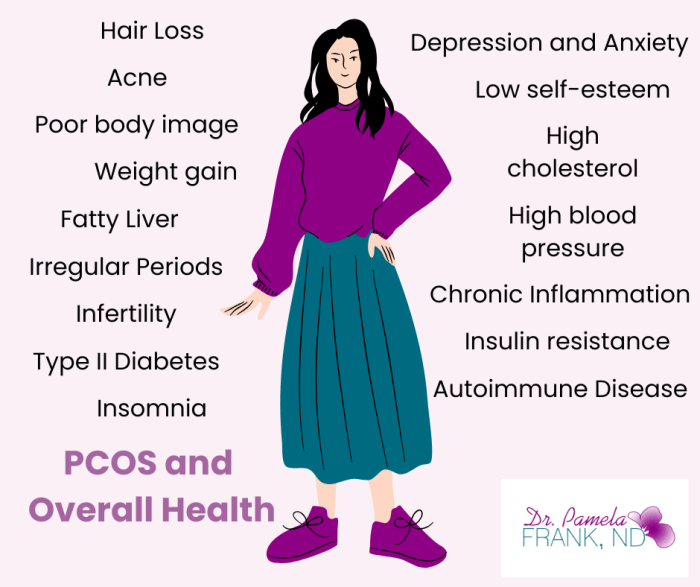
Polycystic Ovary Syndrome (PCOS) is often misunderstood or ignored as a condition that only affects periods or fertility. In reality, its impact is far more widespread, influencing metabolic, hormonal, cardiovascular, dermatological, and psychological health. PCOS is not just a reproductive disorder; it is a complex, lifelong condition that affects the entire body. Let’s explore the impact of PCOS and overall health.
PCOS, Hormones and Ovulation
PCOS is fundamentally an ovulatory disorder. People with PCOS may not ovulate regularly, or at all, due to hormonal imbalances. Elevated androgens (male hormones such as testosterone, DHEAs, and/or Dihydrotestosterone) and insulin resistance are often key players. These hormonal shifts prevent the release of a mature egg each month, resulting in irregular or absent periods, difficulty conceiving, and a range of other symptoms.
But the hormonal chaos doesn’t stop there. PCOS is also linked to elevated luteinizing hormone (LH), low or normal follicle-stimulating hormone (FSH), increased estrogen, and sometimes elevated prolactin. These disruptions can lead to acne, excess facial or body hair, scalp hair thinning, and mood changes.
PCOS and Metabolic Health
Insulin resistance affects 50% to 70% of individuals with PCOS, even those who are not overweight. Insulin is a hormone that facilitates the entry of glucose into cells for energy. When cells become resistant to insulin, the body compensates by producing more of it, which can increase androgen production and further impair ovulation.
This resistance can also contribute to weight gain, difficulty losing weight, increased appetite, and a higher tendency towards sugar cravings. Although up to 40% of people with PCOS can be thin and yet still insulin resistant. Long-term, insulin resistance significantly raises the risk of developing type 2 diabetes, metabolic syndrome, and non-alcoholic fatty liver disease (NAFLD).
References:
- Dunaif A. (1997). Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis. Endocrine Reviews, 18(6), 774-800.
- Lim SS, et al. (2012). Overweight, obesity and central obesity in women with polycystic ovary syndrome: a systematic review and meta-analysis. Human Reproduction Update, 18(6), 618–637.
PCOS and Mental Health
The psychological burden of PCOS is often underestimated. Individuals with PCOS are at a significantly higher risk of depression, anxiety, low self-esteem, and disordered eating. Hormonal imbalances, body image issues, and the frustration of dealing with persistent symptoms all play a role.
Studies have found that women with PCOS are up to three times more likely to experience depression than those without the condition. Sleep disturbances, often related to insulin resistance and hormonal imbalance, further exacerbate mental health struggles.
References:
- Dokras A, et al. (2011). Increased prevalence of anxiety symptoms in women with polycystic ovary syndrome: systematic review and meta-analysis. Fertility and Sterility, 97(1), 225-230.
- Cooney LG, et al. (2017). Depression and anxiety in women with polycystic ovary syndrome: current perspectives. International Journal of Women’s Health, 9, 567–577.
PCOS and Cardiovascular Health
Even though PCOS is diagnosed during the reproductive years, its impact on long-term cardiovascular health is significant. This impact extends beyond the reproductive years, through menopause. Insulin resistance, obesity, inflammation, and dyslipidemia (abnormal cholesterol levels) are all common in PCOS and known risk factors for cardiovascular disease.
Women with PCOS have been shown to have higher rates of hypertension, elevated LDL (“bad” cholesterol), lower HDL (“good” cholesterol), and increased triglycerides, even at a young age.
References:
PCOS, Inflammation and Immune Health
Chronic low-grade inflammation is another hallmark of PCOS. Inflammation contributes to insulin resistance and cardiovascular risk and may play a role in the development of ovarian dysfunction. Research also suggests a possible link between PCOS and autoimmune conditions, though this connection requires further exploration.
Beyond the Body: Social and Economic Costs
PCOS also comes with social and financial burdens. Many individuals with PCOS undergo years of medical appointments, fertility treatments, or dermatological procedures. The emotional toll of navigating a misunderstood and often dismissed condition adds to the cost, both literally and figuratively.
PCOS and Overall Health: Conclusion
PCOS is much more than missed periods or difficulty getting pregnant. It affects nearly every system in the body and can significantly reduce quality of life. The good news? With early diagnosis, lifestyle modifications, and a personalized treatment plan, it can be effectively managed.
Empowering individuals with PCOS starts with expanding our understanding. By recognizing its full impact, we can move beyond a narrow view of PCOS and provide the vital, holistic support that people genuinely need.