PCOS is complicated. There are different PCOS Types. It’s not a “one size fits all” kind of condition. It’s a spectrum, meaning every person with PCOS can experience it differently. Today, we’re delving into the intricacies of this complex condition and why understanding its spectrum is crucial to managing it more effectively.
What is PCOS?
Breaking Down the Acronym
PCOS stands for Polycystic Ovary Syndrome, but here’s the kicker – many people with PCOS don’t have cysts on their ovaries. And those who do? The cysts aren’t harmful; they’re just a symptom of hormone imbalance. Confused yet? You’re not alone.
PCOS Is More Than Missed Periods
Sure, irregular periods are often the first clue, but PCOS can show up in many ways: acne that won’t quit, unwanted facial hair, sudden weight gain, or struggles with fertility. It’s not just a period problem – it’s a hormone problem.
The PCOS Spectrum Concept: Not One-Size-Fits-All
Classic vs. Non-Classic PCOS
Classic PCOS often ticks all the boxes – irregular cycles, high androgens, and cystic ovaries. But non-classic types might have only one or two signs. Some people still ovulate, others don’t. Some have insulin issues, others don’t.
PCOS Types: Different Presentations, Different Struggles
Imagine PCOS like a playlist. Everyone’s symptoms are a different mix. Your friend might struggle with acne and weight gain. You? Perhaps your periods are regular, but you’re experiencing hair loss. That’s why the treatment of different PCOS types should never be a copy-and-paste approach.
Common Symptoms Across the PCOS Spectrum
Irregular Periods and Ovulation
The most well-known symptom. Skipping periods or having long cycles often signals that ovulation isn’t happening regularly – bad news if you’re trying to conceive.
Acne, Hair Loss, and Hirsutism
Blame it on the androgens – aka male hormones like testosterone. High levels can cause deep cystic acne, thinning scalp hair, or coarse hair in places you’d rather not have it.
Weight Struggles and Insulin Resistance
Insulin resistance is sneaky. Slim people can have it. It makes the body store fat more easily and disrupts hormone levels. No wonder PCOS makes weight loss feel impossible.
Underlying Drivers: What’s Going On Beneath the Surface?
Insulin Resistance
More than half of the people with PCOS have it. Insulin resistance means your cells don’t respond well to insulin, so your pancreas pumps out more. This can increase androgen levels and worsen symptoms.
Elevated Androgens
High testosterone is often a hallmark. It throws off the hormone balance that helps with ovulation and can trigger skin and hair issues.
Chronic Inflammation
Low-grade inflammation is common in PCOS. It contributes to insulin resistance and hormonal imbalance. You might not feel inflamed, but it’s there, operating behind the scenes.
Genetics and Family History
PCOS runs in families. If your mother, sister, or aunt has it, there is a higher chance that you will too. But lifestyle still plays a role too; genes load the gun, and diet and lifestyle pull the trigger.
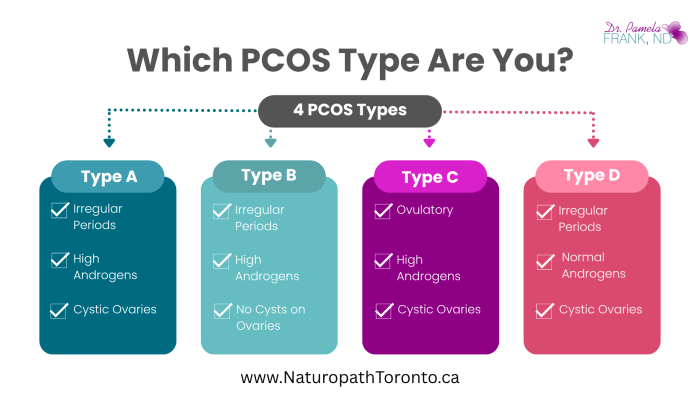
PCOS Phenotypes: The 4 Main PCOS Types
Type A: Classic PCOS (All 3 Criteria)
Irregular periods, high androgens, and polycystic ovaries. This type is the most well-researched and usually the most symptomatic.
Type B: Hyperandrogenic + Irregular Cycles
You’ve got the hormonal imbalance and cycle issues, but your ovaries look fine on ultrasound. Still PCOS.
Type C: Ovulatory PCOS
This one’s sneaky. You ovulate regularly but have signs of high androgens and polycystic ovaries. Often missed by doctors.
Type D: Non-Hyperandrogenic PCOS
Irregular periods and cystic ovaries, but androgen levels are normal. Less common, but still valid.
The Emotional and Mental Load
Anxiety and Depression
Hormones affect mood. The rollercoaster of symptoms, plus the uncertainty, can take a serious toll on mental health.
Body Image and Self-Esteem
Let’s be honest – dealing with acne, weight gain, or facial hair can be demoralizing. It’s not just physical. It’s emotional, too.
Getting Diagnosed: Why It’s Tricky
The Rotterdam Criteria
You need two out of three:
- Irregular periods
- High androgens
- Polycystic ovaries
Seems simple, but it’s not. Many people go years without a proper diagnosis.
Overlap with Other Conditions
PCOS can mimic hypothyroidism, high prolactin, and even adrenal disorders. That’s why it’s crucial to rule those out before jumping to conclusions.
Treatment: Tailoring to the Person, Not the Syndrome
Lifestyle Changes: Food, Movement, and Sleep
Even small tweaks matter. Balancing blood sugar, exercising regularly, and getting quality sleep can help shift your hormones in the right direction.
Supplements and Herbal Support for Different PCOS Types
Think inositol for insulin, spearmint tea for androgens, zinc for acne, and NAC for inflammation. But always check with your healthcare provider first. Many other options may be more appropriate than these in your specific circumstances.
Medications and Medical Interventions
Sometimes meds like metformin or hormonal birth control can help—but they’re tools, not cures. It’s about what works for you.
Why Early Diagnosis Matters
Preventing Long-Term Complications
PCOS increases the risk of diabetes, heart disease, and uterine cancer. The earlier it’s managed, the better the outcome.
Preserving Fertility
Early support can improve ovulation and protect your chances of getting pregnant later, if and when you’re ready.
Final Thoughts: Embracing Your PCOS Journey
PCOS is a journey, not a destination. It’s not just about periods or fertility—it’s about your whole health. And while the spectrum and different PCOS types can feel overwhelming, it also means there’s room for personalized care, healing, and hope.
FAQs
1. Can you have PCOS if your periods are regular?
Yes! Some types of PCOS involve regular ovulation. You might still have high androgens or polycystic ovaries.
2. Is weight gain inevitable with PCOS?
Not at all. While PCOS can make it harder to maintain weight, it’s absolutely possible with the right strategies.
3. Does everyone with PCOS need medication?
Nope. Some manage PCOS entirely with lifestyle, supplements, and support. Others benefit from meds. It’s personal.
4. Can PCOS go away?
You can manage symptoms and even reverse many of them—but PCOS is a lifelong tendency, not something that “goes away.”
5. What doctor should I see for PCOS?
Start with a family doctor or OB-GYN, but many find great help with endocrinologists or naturopathic doctors who understand the full spectrum.
PCOS Types References
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. (2004). Revised 2003 consensus on diagnostic criteria and long-term health risks related to PCOS.
- Azziz R, Sanchez LA, Knochenhauer ES, Moran C, Lazenby J, Stephens KC, Taylor K, Boots LR. Androgen excess in women: experience with over 1000 consecutive patients. J Clin Endocrinol Metab. 2004 Feb;89(2):453-62. doi: 10.1210/jc.2003-031122. PMID: 14764747.
- Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, Piltonen T, Norman RJ; International PCOS Network. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2018 Sep 1;33(9):1602-1618. doi: 10.1093/humrep/dey256. Erratum in: Hum Reprod. 2019 Feb 1;34(2):388. doi: 10.1093/humrep/dey363. PMID: 30052961; PMCID: PMC6112576.
- Legro RS, Arslanian SA, Ehrmann DA, Hoeger KM, Murad MH, Pasquali R, Welt CK; Endocrine Society. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013 Dec;98(12):4565-92. doi: 10.1210/jc.2013-2350. Epub 2013 Oct 22. Erratum in: J Clin Endocrinol Metab. 2021 May 13;106(6):e2462. doi: 10.1210/clinem/dgab248. PMID: 24151290; PMCID: PMC5399492.
- Lim SS, Hutchison SK, Van Ryswyk E, Norman RJ, Teede HJ, Moran LJ. Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database of Systematic Reviews 2019, Issue 3. Art. No.: CD007506. DOI: 10.1002/14651858.CD007506.pub4. Accessed 26 July 2025.