Chronic inflammation is increasingly recognized as a driver of metabolic, hormonal, immune, and degenerative disease. While inflammation is often discussed in terms of immune cells and cytokines, a less visible, but critically important player sits at the center of this process: cellular energy metabolism.
The organelles responsible for energy production do far more than generate ATP. They regulate oxidative balance, immune signalling, stress responses, and programmed cell death. When these systems falter, inflammatory pathways can become dysregulated, creating a self-perpetuating cycle of energy failure and immune activation.
What mitochondrial dysfunction actually means
Mitochondrial dysfunction refers to impaired performance of the cell’s bioenergetic machinery. In research settings, this may involve one or more of the following abnormalities:
- Reduced efficiency of ATP generation
- Impaired electron transport chain activity
- Excess production of reactive oxygen species (ROS)
- Damage to mitochondrial membranes
- Disrupted fusion and fission dynamics
- Inadequate mitophagy, the process that removes damaged organelles
Rather than being an isolated energy issue, compromised bioenergetic function alters how cells respond to stress, infection, and metabolic demand. Immune cells, in particular, rely on tightly regulated energy signalling to switch between inflammatory and resolution states. When this regulation breaks down, inflammation can persist beyond its functional purpose.
How impaired cellular energy systems promote inflammation
1. Excess oxidative stress as an inflammatory trigger
Under healthy conditions, mitochondria generate small amounts of ROS that act as signalling molecules. When energy production becomes inefficient, ROS generation can rise sharply. Elevated mitochondrial-derived oxidative stress can activate inflammatory transcription factors and damage surrounding cellular structures, amplifying immune responses.
2. Release of mitochondrial danger signals
Because mitochondria evolved from bacteria, some of their components resemble microbial molecules. When cellular energy organelles are damaged, substances such as mitochondrial DNA (mtDNA) can escape into the cytosol or circulation. The immune system may interpret these as danger signals, triggering innate immune activation even in the absence of infection.
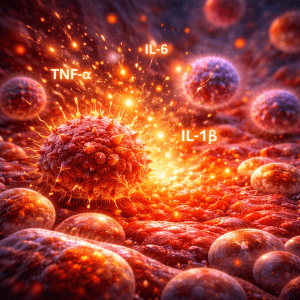
3. Activation of the NLRP3 inflammasome
One of the most studied links between bioenergetic stress and inflammation is the NLRP3 inflammasome. This immune complex plays a central role in producing inflammatory cytokines such as IL-1β and IL-18. Research shows that excess mitochondrial ROS, leaked mtDNA, and impaired clearance of damaged energy organelles can all promote inflammasome activation.
Common causes of mitochondrial dysfunction
In most people, reduced mitochondrial efficiency develops gradually and reflects multiple overlapping stressors, including:
- Aging, which is associated with declining mitochondrial quality control and low-grade systemic inflammation
- Insulin resistance, obesity, and metabolic syndrome, which place sustained stress on cellular energy pathways
- Physical inactivity leads to reduced mitochondrial density and adaptability
- Circadian rhythm disruption and poor sleep, which impair metabolic-immune coordination
- Chronic psychological stress indirectly increases oxidative and inflammatory load
- Environmental exposures, including smoking, air pollution, and certain toxins
- Persistent immune activation or infection, which increases oxidative burden and inflammasome signalling
- Micronutrient insufficiencies, particularly nutrients required for electron transport and antioxidant defence
Natural interventions shown to support mitochondrial health
Claims about “reversing” mitochondrial dysfunction must be precise. However, a growing body of research demonstrates that specific lifestyle and nutritional interventions can improve mitochondrial efficiency, resilience, and signalling, often accompanied by reductions in inflammatory markers.
Exercise: the most powerful mitochondrial intervention
Regular physical activity, particularly aerobic and interval-based training, stimulates mitochondrial biogenesis and improves oxidative phosphorylation efficiency. These adaptations are mediated by signalling pathways involving PGC-1α and are consistently observed across age groups and metabolic states.
Even moderate, consistent movement can meaningfully enhance cellular energy capacity.
Calorie modulation and intermittent fasting
Human trials show that calorie restriction, intermittent fasting, and time-restricted eating can improve mitochondrial-related immune and metabolic signalling, particularly in individuals with obesity or insulin resistance. Changes in circulating immune cells have been observed, suggesting systemic benefits.
These benefits appear to stem from reduced metabolic stress and improved bioenergetic flexibility.
Omega-3 fatty acids (EPA and DHA)
Omega-3 intake has been shown to influence mitochondrial membrane composition and improve aspects of cellular energy kinetics in skeletal muscle. Emerging research also links omega-3s to improved mitochondrial bioenergetics in immune cells, with downstream anti-inflammatory effects.
Coenzyme Q10 (CoQ10)
CoQ10 plays a central role in the electron transport chain and acts as a lipid-soluble antioxidant. Meta-analyses of randomized controlled trials show improvements in inflammatory and oxidative stress markers with supplementation, particularly in populations with elevated oxidative burden.
Curcumin
Curcumin’s anti-inflammatory effects are well established, but newer research suggests it may also influence mitochondrial dynamics and stress signalling, contributing to improved inflammatory regulation in specific contexts.
NRF2-activating compounds (e.g., sulforaphane)
Activation of the NRF2 pathway enhances your internal antioxidant defences and cellular stress resilience. Sulforaphane, found in broccoli sprouts, is one of the most studied dietary NRF2 activators and has been linked to protection of mitochondrial integrity under oxidative stress.
Melatonin (context-specific)
Beyond its role in sleep regulation, melatonin has been shown in human studies to influence mitochondrial enzyme activity and oxidative balance. Its effects are highly context-dependent, making individualized use necessary.
Reducing inflammation by supporting cellular energy
Taken together, the research supports a simple, evidence-aligned approach:
- Move regularly to stimulate mitochondrial biogenesis and efficiency
- Reduce metabolic overload through sustainable nutrition strategies
- Protect circadian rhythms and sleep quality
- Use targeted nutraceuticals when appropriate, based on individual needs and clinical context
Rather than chasing inflammation in isolation, improving cellular energy resilience addresses a root mechanism that influences immune balance, metabolic health, and long-term disease risk.
Mitochondria References
- Zong Y, Li H, Liao P, Chen L, Pan Y, Zheng Y, Zhang C, Liu D, Zheng M, Gao J. Mitochondrial dysfunction: mechanisms and advances in therapy. Signal Transduct Target Ther. 2024 May 15;9(1):124. doi: 10.1038/s41392-024-01839-8. PMID: 38744846; PMCID: PMC11094169.
- Holley, C. L., & Schroder, K. (2020). The rOX-stars of inflammation: Links between the inflammasome and mitochondrial meltdown. Clinical & Translational Immunology, 9(2), e01109. https://doi.org/10.1002/cti2.1109
- Mishra SR, Mahapatra KK, Behera BP, Patra S, Bhol CS, Panigrahi DP, Praharaj PP, Singh A, Patil S, Dhiman R, Bhutia SK. Mitochondrial dysfunction as a driver of NLRP3 inflammasome activation and its modulation through mitophagy for potential therapeutics. Int J Biochem Cell Biol. 2021 Jul;136:106013. doi: 10.1016/j.biocel.2021.106013. Epub 2021 May 19. PMID: 34022434.
- Mølmen KS, Almquist NW, Skattebo Ø. Effects of Exercise Training on Mitochondrial and Capillary Growth in Human Skeletal Muscle: A Systematic Review and Meta-Regression. Sports Med. 2025 Jan;55(1):115-144. doi: 10.1007/s40279-024-02120-2. Epub 2024 Oct 10. PMID: 39390310; PMCID: PMC11787188.
- Guevara-Cruz M, Hernández-Gómez KG, Condado-Huerta C, González-Salazar LE, Peña-Flores AK, Pichardo-Ontiveros E, Serralde-Zúñiga AE, Sánchez-Tapia M, Maya O, Medina-Vera I, Noriega LG, López-Barradas A, Rodríguez-Lima O, Mata I, Olin-Sandoval V, Torres N, Tovar AR, Velázquez-Villegas LA. Intermittent fasting, calorie restriction, and a ketogenic diet improve mitochondrial function by reducing lipopolysaccharide signalling in monocytes during obesity: A randomized clinical trial. Clin Nutr. 2024 Aug;43(8):1914-1928. doi: 10.1016/j.clnu.2024.06.036. Epub 2024 Jul 5. PMID: 39003957.
- Spadaro O, Youm Y, Shchukina I, Ryu S, Sidorov S, Ravussin A, Nguyen K, Aladyeva E, Predeus AN, Smith SR, Ravussin E, Galban C, Artyomov MN, Dixit VD. Caloric restriction in humans reveals immunometabolic regulators of health span. Science. 2022 Feb 11;375(6581):671-677. doi: 10.1126/science.abg7292. Epub 2022 Feb 10. PMID: 35143297; PMCID: PMC10061495.
- Herbst EA, Paglialunga S, Gerling C, Whitfield J, Mukai K, Chabowski A, Heigenhauser GJ, Spriet LL, Holloway GP. Omega-3 supplementation alters mitochondrial membrane composition and respiration kinetics in human skeletal muscle. J Physiol. 2014 Mar 15;592(6):1341-52. doi: 10.1113/jphysiol.2013.267336. Epub 2014 Jan 6. PMID: 24396061; PMCID: PMC3961091.
- Dabbaghi Varnousfaderani S, Musazadeh V, Ghalichi F, Kavyani Z, Razmjouei S, Faghfouri AH, Ahrabi SS, Seyyed Shoura SM, Dehghan P. Alleviating effects of coenzyme Q10 supplements on biomarkers of inflammation and oxidative stress: results from an umbrella meta-analysis. Front Pharmacol. 2023 Aug 8;14:1191290. doi: 10.3389/fphar.2023.1191290. PMID: 37614320; PMCID: PMC10442645.
- Hou D, Liao H, Hao S, Liu R, Huang H, Duan C. Curcumin simultaneously improves mitochondrial dynamics and myocardial cell bioenergy after sepsis via the SIRT1-DRP1/PGC-1α pathway. Heliyon. 2024 Mar 28;10(7):e28501. doi: 10.1016/j.heliyon.2024.e28501. PMID: 38586339; PMCID: PMC10998060.
- Dinkova-Kostova AT, Copple IM. Advances and challenges in therapeutic targeting of NRF2. Trends Pharmacol Sci. 2023 Mar;44(3):137-149. doi: 10.1016/j.tips.2022.12.003. Epub 2023 Jan 9. PMID: 36628798.